Acadia Healthcare is committed to advancing approaches in mental health and addiction treatment. We continually work to enhance the quality of care we provide and to support meaningful progress for the individuals we serve. By incorporating measurement‑based care into our practices, we aim to strengthen consistency, transparency, and clinical rigor across our treatment services.
What Is Measurement-Based Care?
As an organization that consistently takes steps to innovate the way mental health and addiction treatment is delivered, Acadia is focused on the use of measurement-based care (MBC).
Measurement-based care is an evidence-based practice that uses routine, structured assessments to guide clinical decision-making and improve treatment outcomes. It is an ongoing process of using validated tools, such as symptom rating scales, quality of life assessments, and patient-reported outcome measures, to track a patient’s progress at the beginning, during and at the conclusion of treatment. It allows clinicians to use real-time data to identify changes in symptoms, adjust treatment plans, and help patients remain engaged in their own care.
In short, key elements of MBC include:
- Patients completing brief, standardized measures at frequent, predetermined intervals
- Clinicians using the results of the assessments to tailor interventions, adjust therapeutic strategies, and intensify care when needed
- Clinicians sharing the results with patients to help them understand their progress and actively participate in treatment
Collecting data on patient progress and therapeutic outcomes is important for treatment fidelity, therapeutic alliance, and patient satisfaction. This approach allows us to have a better understanding of what works for our patients so that they can achieve successful treatment outcomes.
Additionally, by monitoring patient responses and recognizing both areas of progress and opportunities for improvement, we are able to continually refine our clinical care to help ensure our services remain responsive, high‑quality, and aligned with the needs of those we serve.
Why Is Measurement-Based Care Important?
The primary purpose of implementing MBC in the treatment process is to facilitate opportunities to further elevate treatment effectiveness and program fidelity. It supports a more data-driven and personalized approach to treatment. By regularly assessing patients’ progress through standardized assessments, clinicians gain real-time insights into what is working and what is not. This not only has the potential to improve outcomes by helping clinicians tailor interventions to individual needs, but it also fosters transparency and collaboration between patients and providers.
MBC can enable better decision-making, enhance accountability, and ultimately lead to more consistent, measurable improvements in behavioral healthcare. It helps bring structure, accountability, and objective information into behavioral health treatment, similar to how vital signs and lab values guide medical care. It supports both individual clinical care and organizational clinical care improvement.
Research consistently shows that MBC leads to better symptom improvement, higher engagement, fewer treatment failures, and the delivery of more efficient and effective care1.
- See Lambert MJ et al., Clin Psychol 2003;10(3):288–301; Krägeloh CU et al., Psychiatr Serv 2015;66(3):224–241; Gondek D et al., Adm Policy Ment Health 2016;43(3):325–343; Williams K et al., Patient-Reported Outcome Measures: Literature Review (Sydney: Australian Commission on Safety and Quality in Health Care; 2016); Tam HE & Ronan K, Clin Psychol Rev 2017;55:41–55; Waldrop J & McGuinness TM, J Psychosoc Nurs Ment Health Serv 2017;55(11):30–35; Shimokawa K et al., J Consult Clin Psychol 2010;78(3):298–311.
Assessments Used in Measurement-Based Care at Acadia
Clinicians at Acadia facilities have access to a core set of assessments that can inform measurement-based care and provide insight into patient needs as treatment progresses so that they can provide measurement-based care and work to address each patient’s needs throughout the course of treatment.
Mental Health Quality of Life (MHQoL)
The MHQoL is a measure of quality of life that assesses various domains including self-image, independence and one’s sense of hope. It is a self-report, seven-item questionnaire that is given to adults age 18 and older.
Patient Health Questionnaire-9 (PHQ-9)
The PHQ-9 is an assessment for adults age 18 and older that is meant to identify those who may have depression based on matching symptoms to diagnostic criteria. This is also able to be used as a continuous measure to assess the severity of depression symptoms at the time treatment begins, throughout the course of the treatment process, and at the conclusion of treatment.
Patient Health Questionnaire-9 for Adolescents (PHQ-A)
The PHQ-A is designed specifically for adolescents ages 11-17. It helps identify children and teens who may have depression, and it is also able to be implemented as a way of measuring the severity of their depressive symptoms when treatment starts, throughout the duration of treatment, and when treatment comes to an end.
Generalized Anxiety Disorder 7-Item Scale (GAD-7)
The GAD-7 is for adults age 18 and older to measure generalized anxiety symptoms. It is a seven-item measure that evaluates excessive anxiety and worry about everyday events and activities.
Severity Measure of Anxiety
The GAD is a 10-item severity measure that assesses adolescents ages 11-17 for anxiety symptoms. The symptoms are assessed on a Likert scale of 0 to 4, and the total score is derived from the average total score.
This list is not exhaustive. In addition to the measurement-based assessments above, clinicians have access to several other assessments that may be used depending on the patient’s clinical presentation, including these additional assessments.
Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5)
The PCL-5 is a posttraumatic stress disorder (PTSD) checklist that includes 20 items that are used to evaluate symptoms of trauma, including avoidance, negative changes in cognition and mood, re-experiencing symptoms, and alterations in arousal and reactivity. The PCL-5 is available to be administered when patient reports that they experienced a significant stressor in their lives. The measure assesses the presence of clinically significant trauma symptoms as well monitors symptom change during and at the end of treatment.
Substance Use Disorder Urge To Use Scale (UTU)
The UTU is a measure that can assess the urge to use a substance. It has been demonstrated to be a valid and reliable instrument in measuring a person’s cravings for substances.
Brief Addiction Monitor (BAM)
The BAM-IOP is a 17-item multidimensional progress monitoring, which helps assess a person’s risk for relapse or worsening severity of SUD symptoms, protective behaviors that support recovery and resistance to relapse, and use of alcohol and other substances.
Clinical Excellence
We believe it is important for patients to understand that the clinical practices in our facilities are guided by a commitment to providing high‑quality, clinically informed care. Through the use of measurement‑based care, we gain clearer insight into each patient’s progress and support a stronger therapeutic relationship. We also aim to have patients feel confident that our approach to treatment is shaped by the goal of delivering care rooted in sound clinical principles and aligned with best practices.
Our Commitment to Our Patients
Our clinical care is guided by a deep commitment to supporting patients throughout their treatment experience. We recognize that seeking help takes courage, and we strive to honor that courage by approaching each individual’s care with compassion, respect, and dedication to their well‑being. We believe that no two healing journeys are identical. Everyone has their own unique experiences, challenges, and goals, and we believe that their treatment plans should reflect that. We don’t rely on one-size-fits-all solutions. Instead, we take the time to listen to each person’s story, understand their needs, and collaborate with them to build a care strategy that meets them where they are.
Compassion is at the heart of the care we deliver, and science, research, and data guide the methods we use. We are committed to using proven clinical approaches that yield tangible results, including:
- Clinically validated therapies: We utilize evidence-based treatment modalities, like cognitive behavioral therapy (CBT) and dialectical behavior therapy (DBT), that are backed by rigorous research.
- Measurable progress: Utilizing measurement-based care allows us to track each person’s progress so that treatment plans can quickly evolve to meet their specific and unique needs
- Best practices: Our clinicians actively strive to incorporate emerging best practices in behavioral health, allowing us to continually strengthen our treatment approach and better support the individuals in our care.
As a connected community of treatment facilities that deliver specialized, whole-person care, we are dedicated to helping our patients thrive. Our mission is to provide compassionate care that improves lives, inspires hope, and elevates communities.

*Determined by MCID score
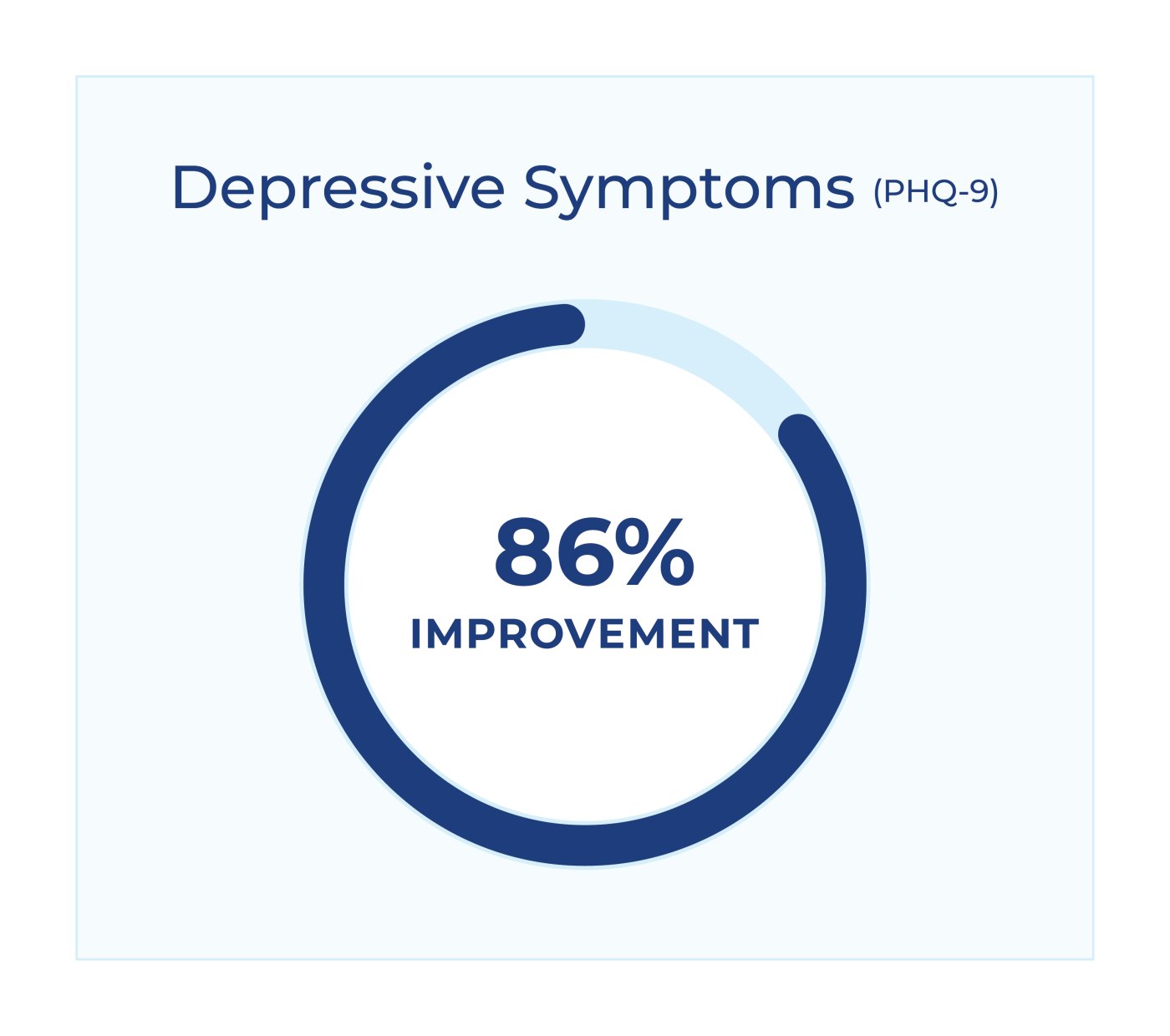
*Determined by MCID score
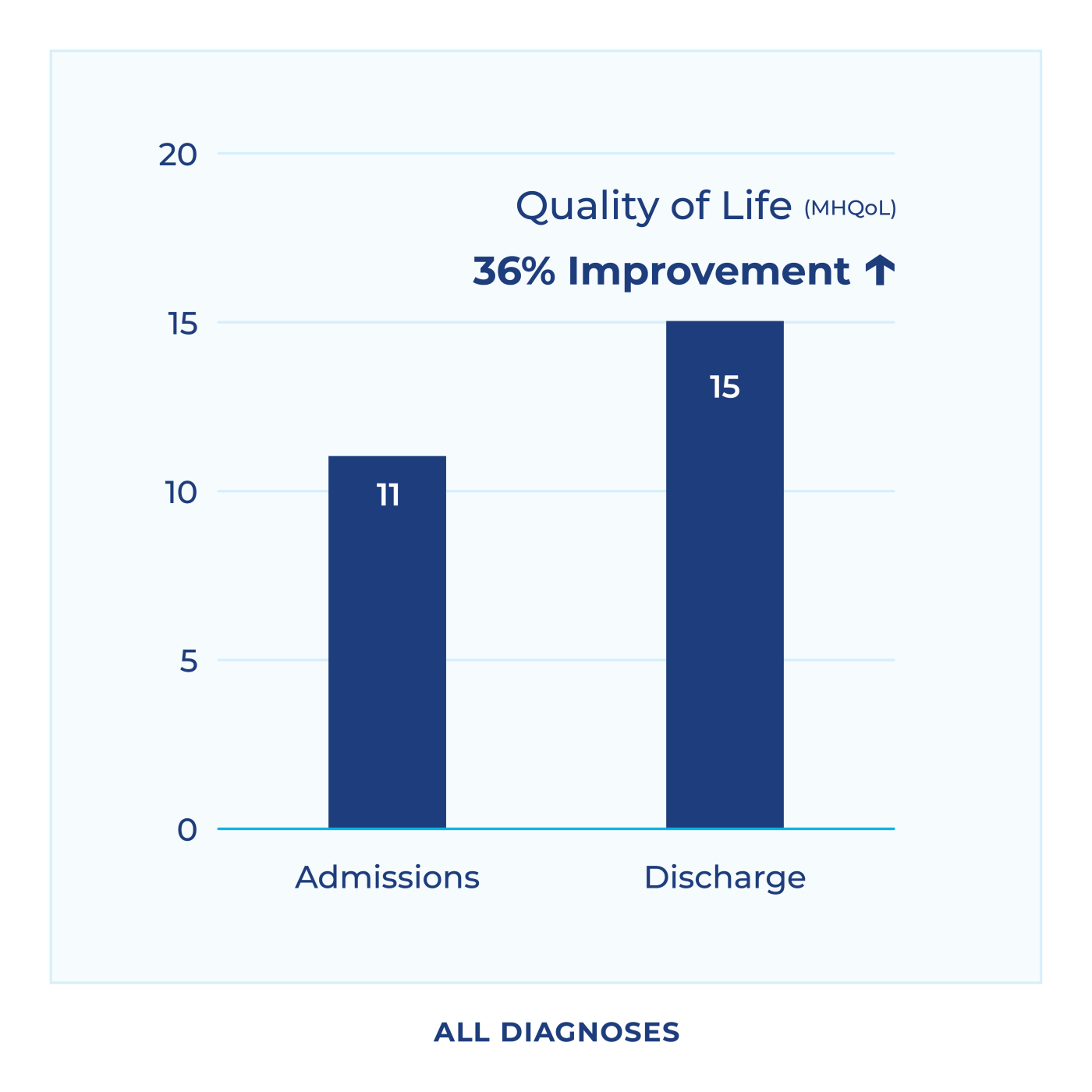
*Improvement reflective of medium effect size. N=9007
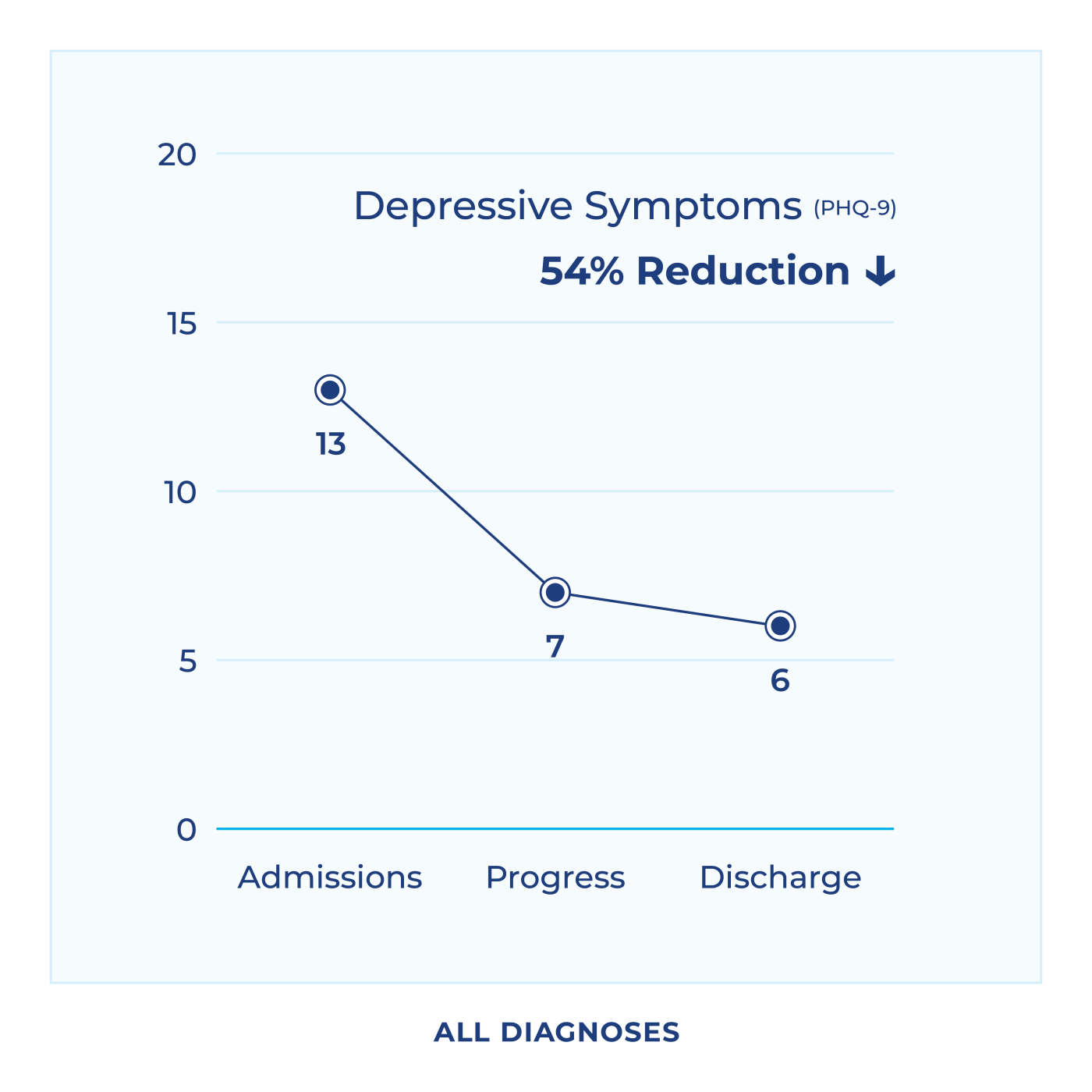
*Reduction reflective of large effect size. N=8992
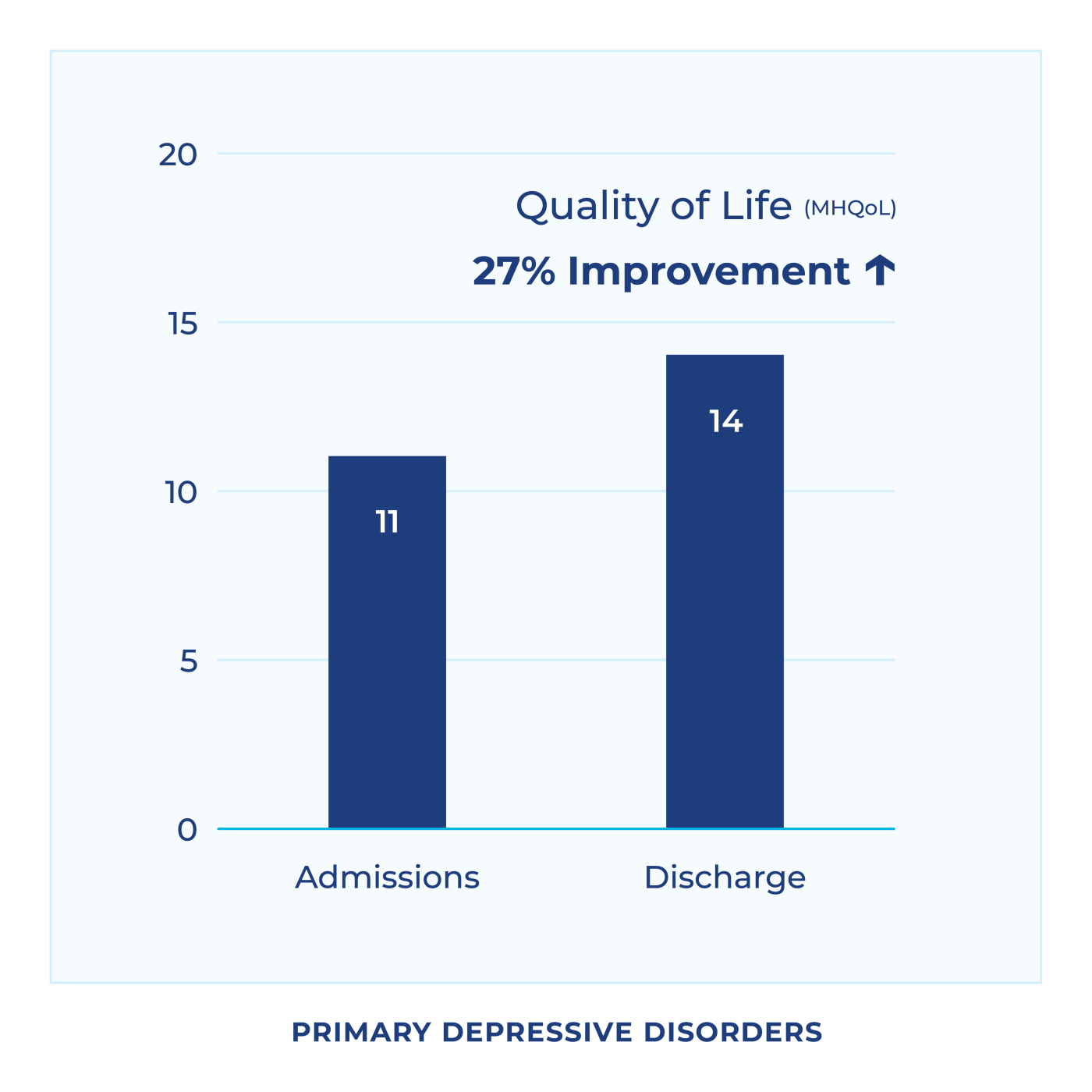
*Improvement reflective of medium effect size. N=2855
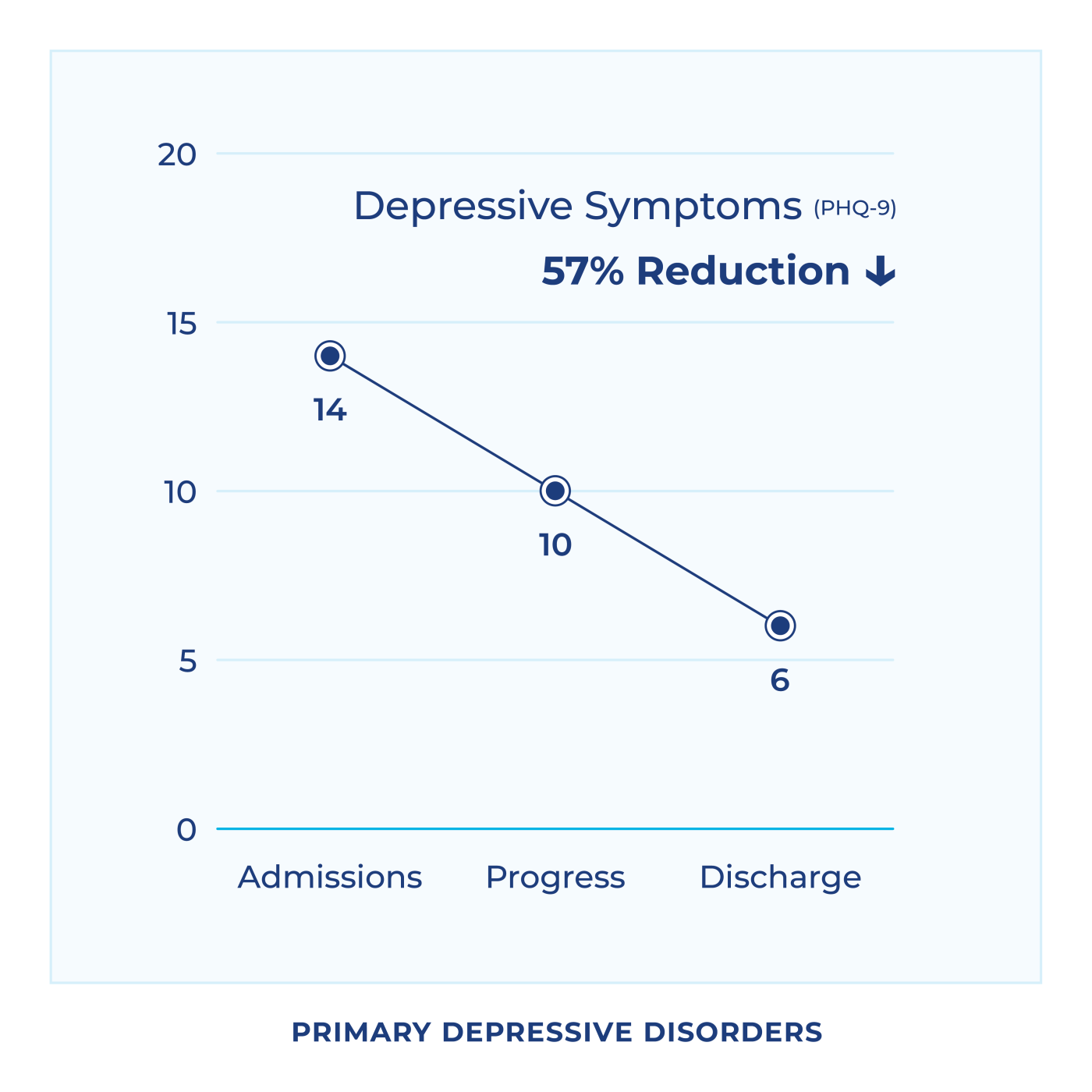
*Reduction reflective of large effect size. N=2877
Data were collected between February 2025 and December 2025 from 33 acute inpatient facilities. Facilities implemented the assessment process at varying dates throughout 2025.
Patients were included in the dataset if they met the following criteria:
- Standardized assessments were available for administration through the electronic medical record (EMR) system at the facility.
- The patient agreed to complete the assessments and/or was deemed capable of doing so.
- The patient was 18 years of age or older.
- The patient did not endorse 0s on all questions on both GAD-7 and PHQ-9 at admissions or discharge.






